This step-by-step guide explains the Ussing chamber experiment—from setup and clamping to data analysis (Isc, TEER, Gt)—so researchers can generate reproducible, publication-quality epithelial transport data.
Quick Summary
- Purpose: Quantify trans-epithelial ion transport and barrier function.
- Best for: Native epithelia or cell monolayers on permeable supports.
- Core readouts: Short-circuit current (Isc), transepithelial resistance (TEER), conductance (Gt).
- Controls: Symmetric buffers, blank insert resistance, and pharmacologic blockers.
- Outcomes: Mechanistic insight into channels (e.g., CFTR, ENaC), transporters, and tight-junction integrity.
When to Use an Ussing Chamber
- To isolate active transepithelial transport (voltage clamp at 0 mV → measure Isc).
- To separate apical vs. basolateral effects of agonists/inhibitors.
- To benchmark barrier quality via TEER and Gt.
- To compare genotypes, media conditions, or drug candidates.
Materials & Setup Checklist
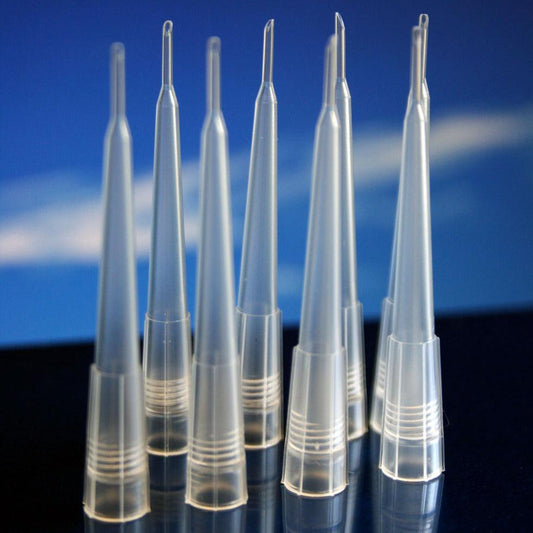
- Ussing chamber system with precision half-cells and temperature control (37 °C typical).
- Voltage/current clamp amplifier and data acquisition software.
- Ag/AgCl electrodes with salt bridges; KCl/agar for junction stability.
- Balanced Ringer or tissue-specific buffers (pH ≈ 7.4; gas as needed).
- Tissue or confluent monolayer on a permeable support (document area A in cm²).
- Water bath or inline heater; peristaltic or gravity perfusion (optional).
- Pharmacology: amiloride (ENaC), forskolin/IBMX (CFTR), bumetanide (NKCC).
- Calibrated pH meter, thermometer, and conductivity/resistance meter.
Core Variables & Typical Ranges
| Variable | Symbol | Typical Target | Notes |
|---|---|---|---|
| Bath temperature | T | 37 °C | Match physiology; maintain ±0.5 °C |
| Bath pH | — | 7.35–7.45 | CO₂/HCO₃⁻ or HEPES-buffered |
| Short-circuit current | Isc | 0.5–200 µA·cm⁻² | Tissue & stimulus dependent |
| Transepithelial resistance | TEER | 200–2,000 Ω·cm² | Subtract blank; × area |
| Conductance | Gt | Low–moderate | Gt = 1/Rt; leak ↑ → Gt ↑ |
Step-by-Step Protocol
- Prepare buffers – warm/aerate both sides, match pH and osmolarity.
- Calibrate electrodes – inspect salt bridges, refill if needed.
- Mount tissue/insert – record area A, remove bubbles along surface.
- Equilibrate baseline – stabilize 5–10 min before stimuli.
- Voltage clamp – set Vt=0 mV; measured current is Isc.
- Pulse for resistance – apply small voltage steps to compute Rt.
- Add pharmacology – dose apical/basolateral; document timing and side.
- Washout & endpoint – save traces, annotate events, export for stats.
Key Equations (Area-Normalized)
R_t (Ω) = ΔV / ΔI TEER (Ω·cm²) = (R_sample – R_blank) × A G_t (S·cm⁻²) = 1 / TEER I_sc (µA·cm⁻²) = I_measured (µA) / A (cm²)
Interpreting the Data
- ΔIsc after agonist → net electrogenic transport via target channels.
- High TEER → intact barrier; low TEER → leak or damage.
- Gt rises with permeabilization; combine with morphology checks.
Recommended Control Sequence
- Baseline clamp at 0 mV (Isc).
- Apical amiloride (ENaC block) → Isc decrease.
- Forskolin/IBMX (stimulate cAMP) → Isc increase via CFTR.
- Bumetanide basolateral (NKCC block) → reduce driving force.
Troubleshooting (Fast Fixes)
| Problem | What You See | Fix |
|---|---|---|
| Drifting baseline | Slow Isc/Vt creep | Rebuild salt bridges; check temperature & pH; remove bubbles. |
| Very low TEER | High Gt, noisy response | Verify insert integrity; replace damaged tissue; subtract blank. |
| No response to agonist | Flat Isc trace | Confirm reagent activity & sidedness; extend equilibration. |
| Spikes when dosing | Transient artifacts | Add slowly; match osmolarity; stir gently. |
Pro Tip: Always report area-normalized data (µA·cm⁻², Ω·cm²) and include blank-subtracted TEER — common reviewer request.
Frequently Asked Questions
What’s the difference between TEER and Isc?
TEER reflects barrier integrity (paracellular). Isc reflects net electrogenic transport (transcellular) under 0 mV clamp.
Do I need CO₂ control?
Use CO₂/HCO₃⁻ buffers if your tissue requires them; otherwise HEPES is fine for short runs if pH is stable.
How long should I equilibrate?
Typically 5–10 minutes after mounting; longer for thicker tissues. Start pharmacology only after a stable baseline.
Reporting Checklist
- Tissue/cell model, passage, confluence criteria
- Exposed area (A), temperature, buffer composition
- Clamp settings, pulse parameters, sampling rate
- Blank resistance, TEER calculation, statistics (n, tests)
- Exact reagent names, concentrations, and sidedness
Next step: If you need a streamlined, high-throughput workflow, consider a chamber system with rapid mounting and stable temperature control to improve repeatability and reduce setup time.
Ready to standardize your Ussing runs? Explore the EasyMount Ussing Chamber and VCC MC8 Voltage Clamp for stable, repeatable data.